First of all, I haven't had my big academic rotation yet. This is the famous "Internal Medicine" rotation (shortened in speech to "IM" for some schools, "I-Med" for us). From what I hear, that is twelve of the most intense weeks of seeing patients, giving presentations, writing notes, being humiliated, and learning the minute mechanics of fluid and medical management.
Did you catch the "being humiliated" in there?
Although I haven't had IMed (and so I feel like I can't really talk about this?), I have had one week of adult inpatient and one week of pediatric inpatient. My attending last week (pediatric) literally said that medicine is taught by shame. "That's how you remember things," he said, "by being put on the spot." I like to think that it's not shame, but responsibility that teaches us. When a person in need, in front of you, is your patient and your attending asks you "how are you going to replace his potassium in light of his serum creatinine?" and you blanch and have no clue, you're going to learn it well and know it next time.
Last week, for instance, I had one week of pediatrics. I got up early to report to the hospital an hour before the attending scheduled "rounds." I was assigned one patient each day, and went to talk with them and examine them and prepare a presentation and admission orders, including IV fluids, drugs and doses, and special nursing instructions. (All of these orders were practice; none were actually carried out except if someone else, e.g. the resident or fourth year, had the same idea/agreed with me and ordered them.)
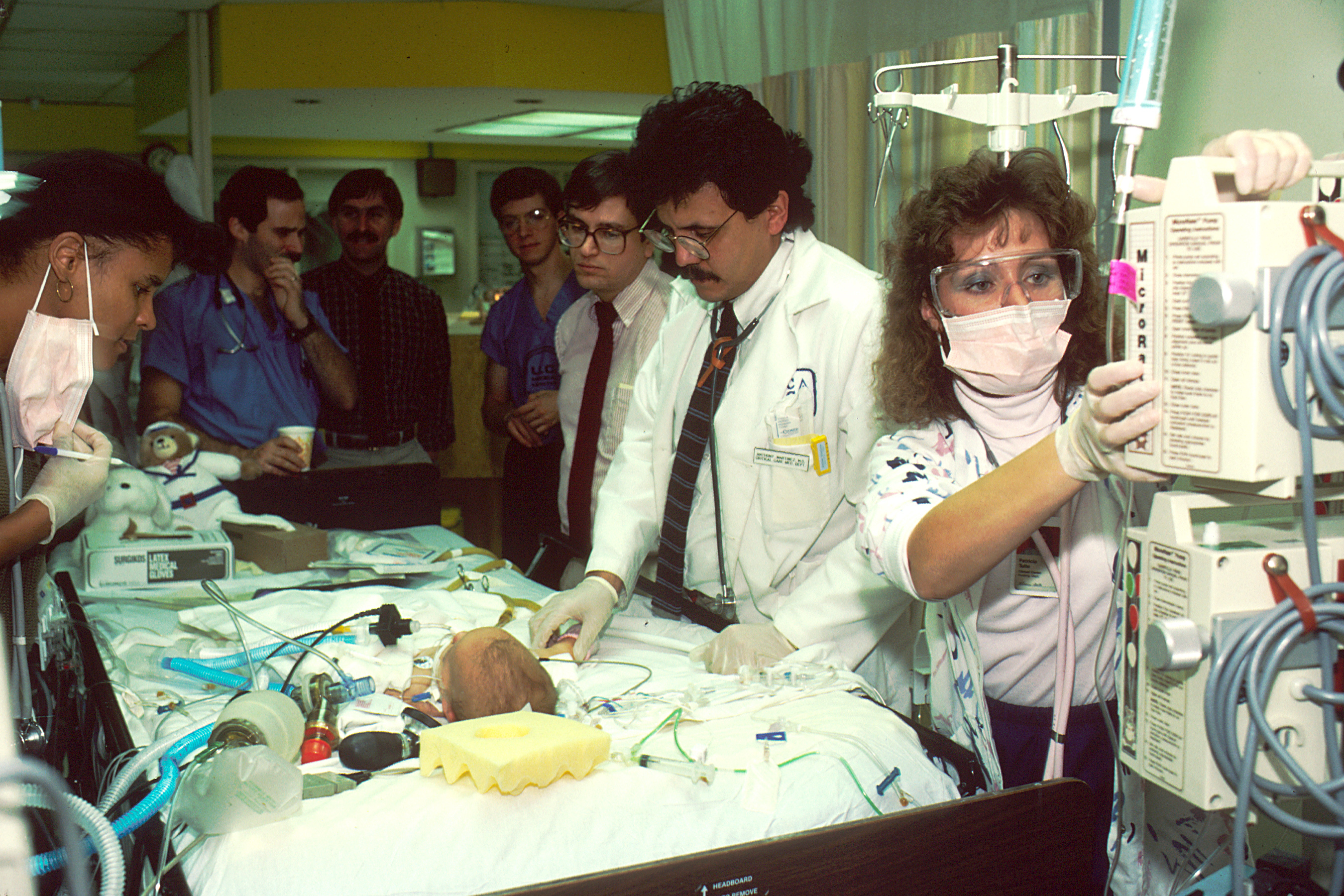 |
| All the people standing behind the attending (who is actually examining the patient) are the med students, etc. A nurse happens to be adjusting the IV fluids at the same time. |
When we came to my patient's room, the attending would face me and say, "go," or I would make eye contact with him and start presenting. "This is a 13-month-old white female who presents with a four-day history of vomiting," I'd rattle off. I'd then describe the history of the present illness (HPI), the pertinent positives and negatives, past medical/surgical history (including birth history for children!), currents meds and allergies, and my objective findings (vital signs, physical exam, labs, and imaging). Then, I state my assessment and plan. "This is a 13-month-old female with gastroenteritis. Plan is replace fluid losses with D5 one-half normal and attempt p.o. challenge today."
And then the education would begin. The attending critiques your presentation skills (if you're really new at this), asks for additional findings (and you better hope you have them), and corrects your plan (you feel awesome if this is all he has to say). Since I am new to this, I got lots of presentation-skills and additional-findings criticism.
Presentation skills are important because we're in medical school to learn to think in an orderly, analytical way about complex problems and not miss things. We're trained to think like a doctor by presenting and writing notes. Presenting skills are also important because communication to colleagues is made quick and safe by a universally-agreed upon format. The format in medicine is:
- Patient ID sentence
- Chief concern
- HPI
- Review of systems (ROS)
- Past medical history (including birth history if pediatrics)
- Past surgical history
- Current meds
- Family history
- Social history
- Allergies
- Vital signs
- Physical exam
- Labs
- Imaging
- Assessment/Plan (A/P)
If your attending asks for additional findings, you are expected to produce them with ease. It looks sort of silly to shuffle through your papers, although that's better than having to say "I don't know" or "I didn't ask." We are supposed to know everything about our patients. (Was there green in the vomit? How far did it fly? What was her serum chloride on Monday? Did we get the results of the 99-technetium scan?) Not knowing a historical detail is not very excusable (it's a rookie mistake, only one level above the presentation skills problems); not knowing a lab result is only slightly less excusable. And one is looked upon as not up to snuff if you miss out on a social issue (e.g. illiteracy, bad home situation, poverty, mental illness, etc).
And A/P criticism, while desired, comes in very different flavors. "I think you forgot a decimal point on her IV fluids" is a lot better than "Now, if you give this potassium, you'll probably put this guy into acute kidney failure. You want that on your hands?" But even so, this is the best tier of criticism, and one hopes to reach it during every presentation.
One problem in this approach is stressed or nervous med students, or those who are shy or have thin skins or fragile self esteem, can get hurt. One girl last week cried! I have been lucky, since TAC and high school accustomed me to faking it till I make it (in terms of confidence, not A/Ps). I also have a good memory for medical knowledge. But I don't like that some med students have to learn by shame and embarrassment. I wish we could all take on responsibilities without being toughened by humiliation. Stay tuned for more about academic medicine in the spring, when I go "on the wards" for twelve weeks of I-Med.
No comments:
Post a Comment